With couples choosing to embrace parenthood later in life and a host of lifestyle diseases attributed to the new age high-stress, low activity way of living, infertility has become an increasingly growing concern. And while science is trying to keep up with the fast-changing needs of parents in waiting, there’s no 100% fail-safe option that guarantees parenthood, unless you’re willing to adopt.
Now, most moms go through the cycle of fertility treatments including hormone pills and injections, IUI, and then IVF as a last resort. But there are many other lesser-known treatments, and Intracytoplasmic Sperm Injection (ICSI) is one.
Dr Asha Baxi, Consultant Obstetrician & Gynaecologist at Motherhood Hospital, explains ICSI in detail and talks about the different factors and the processes involved in the treatment.
1. What is the ICSI treatment for infertility?

ICSI or Intracytoplasmic Sperm Injection is a process that is done to encourage pregnancy in women. Before fertilisation, the head of the sperm must get attached to the outside of the egg. The sperm then pushes through the outer layer into the inside of the egg where fertilisation occurs. In some cases, the outer layer is too thick or hard for the sperm to penetrate or in other cases, the sperm may not be able to swim. In such instances, ICSI or IVF procedures are implemented. ICSI is a type of in-vitro fertilization procedure in which a single sperm cell is injected into the cytoplasm of the egg. It is a technique that is used to prepare the gametes in order to obtain the embryos that may be transferred to a maternal uterus, thus encouraging pregnancy.
2. How is ICSI different from IVF?
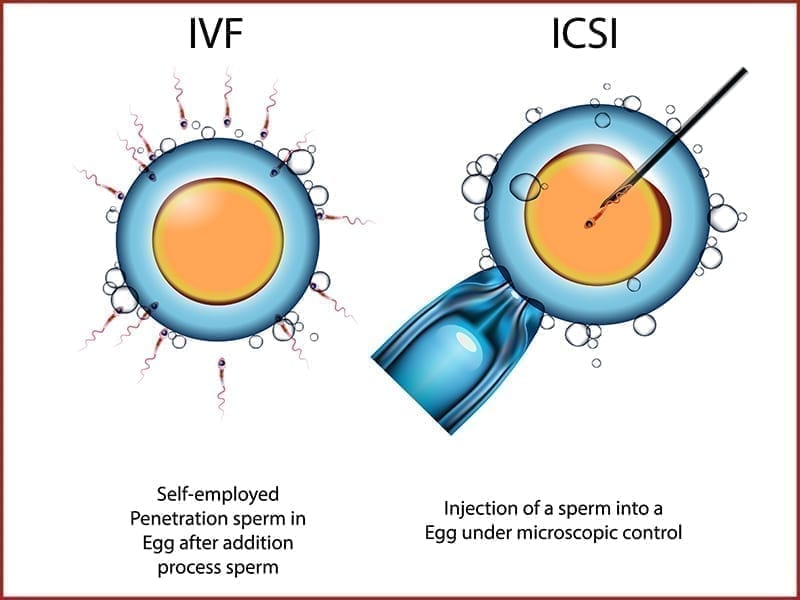
There are two types of treatments to encourage fertility. They are IVF (In Vitro Fertilisation) and ICSI (Intracytoplasmic Sperm Injection). The key difference between the IVF and the ICSI procedures is that in the IVF procedure multiple sperms are collected and left in a petri dish to fertilise. Meanwhile, the ICSI procedure is done to directly inject the sperm into the egg.
3. What factors determine whether one is eligible or should opt for this treatment?

This procedure can also be used for couples who have gone through poor or no fertilisation rates through IVF.
“Intracytoplasmic Sperm Injection is generally recommended to couples who have been diagnosed with male fertility issues. This includes low sperm count, low sperm morphology or motility, anti-sperm antibodies, or anyone who has gone through a vasectomy or an unsuccessful vasectomy reversal.”
4. Is ICSI more successful than IVF?
Fertilisation and implantation rates were significantly higher in IVF compared to the people who went through the ICSI procedure. Chemical and clinical pregnancy rates are statistically higher in those who went through the IVF procedure compared to ICSI. Although the use of ICSI has been estimated as a highly advanced procedure it does not improve fertilisation, implantation and chemical rates, and is not recommended in non-male factor, normozoospermic patients.
5. What is the difference between ICSI and PICSI?

Physiological Intracytoplasmic Sperm Injection (PISI) is essentially an extended technique of ICSI. This involves a functional test for sperm, to aid in their selection for ICSI. The test is based on the sperm’s ability to bind itself to Hyaluron (HA), which mimics the natural binding of mature sperm to oocytes (eggs). Here the prepared sperm is added to a special dish containing Hyaluron at the bottom. The sperms that bind themselves to the Hyaluron are isolated and selected from for ICSI.
6. Are collection of eggs from the woman or sperm retrieval from the man for the ICSI treatment painful?
Usually, sperm is collected through ejaculation. For men who have undergone a vasectomy, a microsurgical vasectomy reversal may be required to restore fertility. When the microsurgical vasectomy reversal does not produce the required results in fertility restoration, needle aspiration or microsurgical sperm retrieval is recommended.
Now, various sperm retrieval techniques are available. These procedures allow the fertility specialist to obtain sperm either by aspirating from the testicle (TESA), or Epididymis (PESA) using a fine needle. Although needle aspiration is a straightforward procedure performed under anaesthesia, it presents a slight risk of pain and swelling. In most cases, this results in minor discomfort. Sperms can also be extracted (TESE) by giving a small incision in the testis and the tubules are examined for the presence of sperms. Even in some cases when FSH levels are high indicating impaired spermatogenesis MicroTESE can pick up small islands of sperms in the tubules. This requires a highly specialised technique which is done under an operating microscope.
In the procedure to collect the eggs, the patient is highly sedated so the chances of experiencing pain are minimal. However, it is common to experience cramps, bloating, constipation, spotting and pain after the removal of eggs. The overall ICSI procedure. however, is not always painful.
7. What is the typical process of ICSI and how long does it take?

The ICSI procedure is a 5-step process that consists of sperm collection, egg collection, sperm injection, observation and implantation.
- Sperm Collection: A semen sample is retrieved from the male partner. This can be collected organically or through a surgical testicular process.
- Egg Collection: Once the semen sample is collected, a selection of mature eggs is collected surgically from the female partner.
- Sperm Injection: Here, a single sperm cell is injected into a healthy egg using a hollow needle to induce fertilisation.
- Observation: Once the egg is fertilised, it becomes an embryo. The embryo is cultured in a laboratory for up to 5 days.
- Implantation: The embryo, that is now 4-5 days old, is transferred to the uterus. After a few days, it embeds itself into the uterine lining. This process is known as implantation.
In the ICSI procedure, a tiny needle called the micropipette is used to inject a single sperm in the centre of the egg. With either traditional IVF or ICSI the fertilised egg, now called the embryo is kept in a laboratory for 1-5 days before it is transferred into the woman’s womb.
8. How is sperm chosen for ICSI? Can the male sperm damage the egg?

It is a well-understood fact that good sperms can produce a healthy embryo. This process injects the sperm into the cytoplasm of an individual oocyte (egg). Initially, a sperm sample is prepared using multiple techniques to eliminate poor quality sperm. The remaining specimen of healthy sperm is then placed under high magnification for a visual inspection by an embryologist. The embryologist picks the “best looking” sperm with a fine glass needle. The embryologist then using a specialised pipette, holds an individually selected oocyte. Using the fine glass needle with the pre-selected sperm, the embryologist punctures through the shell of the oocyte into the cytoplasm. The sperm is slowly and gently injected, and the needle removed.
“One of the most immediate concerns with ICSI is that during the fertilisation process, some eggs might get damaged. Today good labs manage to achieve fertilisation in 70%-80% of the eggs inseminated, meanwhile only damaging 5% of the good quality eggs during the process.”
9. Are ICSI pregnancies high risk? Does ICSI increase risk of miscarriage?
ICSI can increase the success rates of IVF, but the procedure comes with considerable risks.
- Damage to embryos: Fertilisation rates with ICSI range from 50%-80% however, not all become fertilised eggs and some eggs are damaged in the process.
- Becoming pregnant with multiples: There is a high chance to get pregnant with multiples when undergoing the ICSI procedure. Couples that have used ICSI with IVF have about a 30-35% chance of having twins and even a 5-10% chance of being conceived with triplets. Carrying multiples increases the chance of developing complications like gestational diabetes, high blood pressure, low amniotic fluid levels, bed rest, caesarean section and premature labour. When pregnant with multiples, the babies are also at a risk for complications such as being born premature, low birth weight, difficulty in breathing due to immature lungs and are more susceptible to infections.
- Birth defects: The ICSI risk of having a baby with abnormalities is very minimal (less than 1%). Some specific birth defects include sex chromosome abnormalities, Hypospadias (a birth defect in boys where the urethra opening is underneath the penis rather than on the tip), Angelman syndrome, and Beckwith-Weidemann syndrome.
Studies have shown miscarriages can happen in the first trimester following ICSI for women over the maternal age of 31 and/or in the presence of tubal block.
10. How expensive is ICSI? What is the cost of this treatment in India?

Fertility and reproductive procedures cost a fortune in other parts of the world. However, it is quite affordable in India, depending on the medical institution and healthcare centre opted for. ICSI is a procedure that works in multiple cycles and each cycle includes additional costs.
The minimum ICSI cost in India is Rs 2,40,000 to Rs 2,50,000 per cycle. This includes standard procedure and traditional techniques. On a bigger budget, one can check out more advanced procedures that allow for higher success rates. Using these high-tech assistive technologies can bring in an additional cost of Rs 1,45,000 to Rs 2,51,000 on the basic cost. Doctors and specialists might also ask for additional costs.
11. Could you share lifestyle and health advisory for couples considering ICSI?
Patients considering ICSI are generally requested to opt for a better lifestyle and healthy lifestyle choices. A switch to a healthy lifestyle related to physical activity, tobacco, alcohol, nutrition, healthy thinking and sleep is a must. Patients are briefed and requested to live a life that is tobacco-free and modifying hazardous drinking patterns.

